Front line health care workers (HCWs) continue to get infected, quarantined, sidelined, hospitalized, and unfortunately suffer and die, both in the US and internationally, because they use PPE that was not designed for Infectious Disease defense. The World Health Organization estimates at least 115,000 health care workers have died from covid.
What Health Care Workers are Using
The U.S. failed to adequately stockpile PPE, creating shortages, which dangerously produced a false belief that any PPE is better than nothing. When one is starving, everything looks edible.
Current PPE assemblies cobble together a hodgepodge of off-the-shelf and disparate parts that were never designed for Infectious Disease use. This typically consists of: general-purpose coveralls (sold for countless applications such as painting, asbestos removal, chemical spills, etc) or a surgical/isolation gown (which is designed to protect a surgical patient, not a doctor), an N95 respirator, a face shield or goggles, disposable gloves, and sometimes a hair net and booties. This construction of availability has countless problems when used in Infectious Disease defense.
To start:
We’ll expand upon some of these problems below. Others will receive deeper attention in the blogs.
Those yellow surgical gowns ...
... are near useless. Protective apparel used in Infectious Disease defense must include a barrier layer that provides some level of protection. A gown that passes ANSI/AAMI PB 70 Level 2 provides low water resistance (resistant to water spray and some resistance to water penetration under constant contact with increasing pressure) - and is the MINIMUM that any health care worker should wear. Some situations present more fluid thread and warrant ANSI/AAMI PB 70 Level 3. Any gown working against Ebola or a bloodborne pathogen must pass ANSI/AAMI PB 70 Level 4, which includes ASTM 1670 (Standard Test Method for Resistance of Materials Used in Protective Clothing to Penetration by Synthetic Blood) and ASTM 1671 (Standard Test Method for Resistance of Materials Used in Protective Clothing to Penetration by Blood-Borne Pathogens). Those yellow gowns pass none of these levels. Infected water, blood, and any pathogens pass through with minimal effort. They are nothing more than PPE theater. Those yellow gowns are low level surgical isolation gowns intended to maintain a sterile environment during surgery - to prevent a nurse's germs and dust from getting into a patient's open hip for example. Surgical gowns were not designed for protection in the opposite direction: to prevent the patient's germs from reaching the nurse. A lock on a front door is designed to prevent passage in one direction - and does little in the opposite direction. The same directional defense also applies to PPE.
Heck, even the ANSI/AAMI PB 70 levels are misguided when measuring infectious disease defense. A surgical gown can pass ANSI/AAMI PB 70 Level 4 - offering the highest protection according to ANSI/AAMI PB 70 - and yet protect none of the mucous membranes, which are priorities for Infectious Disease defense. That's like a five star crash rating for a car with no brakes.
What Health Care Workers are Using
The U.S. failed to adequately stockpile PPE, creating shortages, which dangerously produced a false belief that any PPE is better than nothing. When one is starving, everything looks edible.
Current PPE assemblies cobble together a hodgepodge of off-the-shelf and disparate parts that were never designed for Infectious Disease use. This typically consists of: general-purpose coveralls (sold for countless applications such as painting, asbestos removal, chemical spills, etc) or a surgical/isolation gown (which is designed to protect a surgical patient, not a doctor), an N95 respirator, a face shield or goggles, disposable gloves, and sometimes a hair net and booties. This construction of availability has countless problems when used in Infectious Disease defense.
To start:
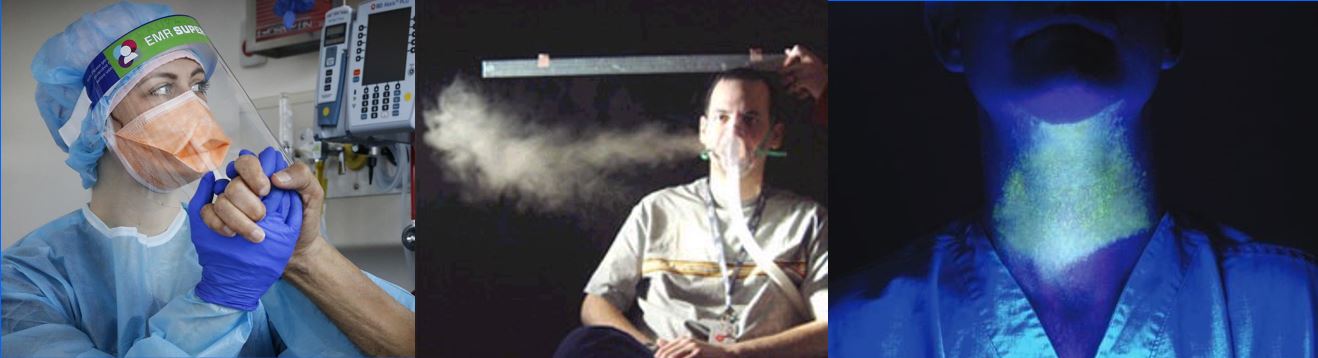
- there are open gaps in the facial area and unprotected eyes, which for aerosol defense is simply useless (see below for more);
- the hodgepodge requires complicated and error prone doffing processes that generate large numbers of self-contaminations;
- the two infected glove doffing conundrum (after removing a first glove, a nurse now has to remove a highly soiled glove with a clean hand); and
- users wear layers of non-breathable materials that trap heat and moisture, leading to perspiration and discomfort, during an already stressful and dangerous situation.
We’ll expand upon some of these problems below. Others will receive deeper attention in the blogs.
Those yellow surgical gowns ...
... are near useless. Protective apparel used in Infectious Disease defense must include a barrier layer that provides some level of protection. A gown that passes ANSI/AAMI PB 70 Level 2 provides low water resistance (resistant to water spray and some resistance to water penetration under constant contact with increasing pressure) - and is the MINIMUM that any health care worker should wear. Some situations present more fluid thread and warrant ANSI/AAMI PB 70 Level 3. Any gown working against Ebola or a bloodborne pathogen must pass ANSI/AAMI PB 70 Level 4, which includes ASTM 1670 (Standard Test Method for Resistance of Materials Used in Protective Clothing to Penetration by Synthetic Blood) and ASTM 1671 (Standard Test Method for Resistance of Materials Used in Protective Clothing to Penetration by Blood-Borne Pathogens). Those yellow gowns pass none of these levels. Infected water, blood, and any pathogens pass through with minimal effort. They are nothing more than PPE theater. Those yellow gowns are low level surgical isolation gowns intended to maintain a sterile environment during surgery - to prevent a nurse's germs and dust from getting into a patient's open hip for example. Surgical gowns were not designed for protection in the opposite direction: to prevent the patient's germs from reaching the nurse. A lock on a front door is designed to prevent passage in one direction - and does little in the opposite direction. The same directional defense also applies to PPE.
Heck, even the ANSI/AAMI PB 70 levels are misguided when measuring infectious disease defense. A surgical gown can pass ANSI/AAMI PB 70 Level 4 - offering the highest protection according to ANSI/AAMI PB 70 - and yet protect none of the mucous membranes, which are priorities for Infectious Disease defense. That's like a five star crash rating for a car with no brakes.

General Purpose Coveralls: really?
We don’t send police officers into deadly situations with painting coveralls. We don’t send firefighters into burning buildings with painting coveralls. Military personnel do not enter firefights wearing painting coveralls. So why do doctors and nurses enter Infectious Disease wards wearing cheap painting coveralls?
Removing contaminated PPE remains a widespread source of infection
The hodgepodge does nothing to facilitate safe doffing. Oppositely, it complicates the process with too many steps, includes error prone tasks, and leads to minimal consistency between users. Used thousands of times per day in an outbreak, health care workers routinely self-contaminate with this disorderly ensemble.
Study videos of health care workers doffing the hodgepodge, and one will see numerous unintended self-contaminations. The number varies with doffing training, but even with training, over 100 self-contaminations per doff is common. Think through numbers when health care workers doff infected PPE thousands or millions of times per day in an outbreak. This is one reason why nations that use the hodgepodge still produced thousands of infected and dead nurses and doctors.
Quality of self-contaminations in the hodgepodge is more troubling than the quantity. One facial self-contamination is more problematic than ten self-contaminations of the shoes. Unfortunately, the hodgepodge leads a person to bring contaminated gloves near – and often in contact with - their face as they remove eye protection (goggle, face shield) and an N95 mask. This generates facial self-contaminations, which are dangerous. If a health care worker is perspiring, then self-contaminations above the eyes can also be problematic.
What’s the point of wearing PPE if health care workers get infected removing it? See more here.
We don’t send police officers into deadly situations with painting coveralls. We don’t send firefighters into burning buildings with painting coveralls. Military personnel do not enter firefights wearing painting coveralls. So why do doctors and nurses enter Infectious Disease wards wearing cheap painting coveralls?
Removing contaminated PPE remains a widespread source of infection
The hodgepodge does nothing to facilitate safe doffing. Oppositely, it complicates the process with too many steps, includes error prone tasks, and leads to minimal consistency between users. Used thousands of times per day in an outbreak, health care workers routinely self-contaminate with this disorderly ensemble.
Study videos of health care workers doffing the hodgepodge, and one will see numerous unintended self-contaminations. The number varies with doffing training, but even with training, over 100 self-contaminations per doff is common. Think through numbers when health care workers doff infected PPE thousands or millions of times per day in an outbreak. This is one reason why nations that use the hodgepodge still produced thousands of infected and dead nurses and doctors.
Quality of self-contaminations in the hodgepodge is more troubling than the quantity. One facial self-contamination is more problematic than ten self-contaminations of the shoes. Unfortunately, the hodgepodge leads a person to bring contaminated gloves near – and often in contact with - their face as they remove eye protection (goggle, face shield) and an N95 mask. This generates facial self-contaminations, which are dangerous. If a health care worker is perspiring, then self-contaminations above the eyes can also be problematic.
What’s the point of wearing PPE if health care workers get infected removing it? See more here.
Full and Uninterrupted Facial Protection
As an airborne threat, covid demands an airborne defense. Covid also leads to multiple hospital procedures that aerosolize infected droplets. Intubations remain a daily task for covid-19 - and a unique PPE challenge. Practitioners commonly use face shields, but these fail to protect aerosols and have been proven to lead to health care worker contamination during intubation.
Another common dangerous aerosolization was discovered in Toronto in 2003, pictured here. BiPap masks apply pressurized air. When the ventilator mask has an imperfect fit (see the CDC graphic for how common this is), a leak in the pressurized mask sends an infected plume that sprays several feet. This is why health care workers need PPE that completely and continuously covers the face with no gaps. Face shields with open bottoms and sides are not enough in this regard since a pressurized plume can easily eddy and vortex under and behind a face shield, into a health care worker’s exposed eyes, leading to infection. A simple face shield futility test: stand behind a 1967 Mustang, wear a face shield, and test if one can smell the unburned gas. Exposed eyes behind a face shield are unprotected when a plume easily eddies around the edges of a face shield.
As an airborne threat, covid demands an airborne defense. Covid also leads to multiple hospital procedures that aerosolize infected droplets. Intubations remain a daily task for covid-19 - and a unique PPE challenge. Practitioners commonly use face shields, but these fail to protect aerosols and have been proven to lead to health care worker contamination during intubation.
Another common dangerous aerosolization was discovered in Toronto in 2003, pictured here. BiPap masks apply pressurized air. When the ventilator mask has an imperfect fit (see the CDC graphic for how common this is), a leak in the pressurized mask sends an infected plume that sprays several feet. This is why health care workers need PPE that completely and continuously covers the face with no gaps. Face shields with open bottoms and sides are not enough in this regard since a pressurized plume can easily eddy and vortex under and behind a face shield, into a health care worker’s exposed eyes, leading to infection. A simple face shield futility test: stand behind a 1967 Mustang, wear a face shield, and test if one can smell the unburned gas. Exposed eyes behind a face shield are unprotected when a plume easily eddies around the edges of a face shield.
Sweating
Some 2020 American practitioners have envied the apparel in this video. Setting aside the doffing problems of that set up, and the questions on efficacy (again, China had thousands of infected health care workers), wearing that many layers of PPE leads to constant perspiration and discomfort.
Sadly, all these problems with the current hodgepodge confirm that these disparate items were not designed to be used for Infectious Disease defense. Health care worker infection will continue as long as the outbreak sends sick people into hospitals. This endangers doctors and nurses, who need real Infectious Disease apparel.
Some 2020 American practitioners have envied the apparel in this video. Setting aside the doffing problems of that set up, and the questions on efficacy (again, China had thousands of infected health care workers), wearing that many layers of PPE leads to constant perspiration and discomfort.
Sadly, all these problems with the current hodgepodge confirm that these disparate items were not designed to be used for Infectious Disease defense. Health care worker infection will continue as long as the outbreak sends sick people into hospitals. This endangers doctors and nurses, who need real Infectious Disease apparel.
